Extreme heat may trigger thousands of hospitalizations in adults with Alzheimer’s
Published: February 5, 2025
This article was originally published by Healio
Key takeaways:
- Study results suggest that each day of extreme heat may contribute to thousands of hospitalizations among those with Alzheimer’s and related dementias.
- Diverse groups had a higher risk for hospitalization.
Older adults with Alzheimer’s disease and related dementias faced a greater risk for hospitalization after being continuously exposed to extreme heat, results from a cohort study showed.
The effects from continuous heat exposure appeared greater in certain diverse populations and climates, while the findings suggest that policymakers “should devise programs to mitigate these risks,” the researchers explained.
Scott W. Delaney, ScD, JD, MPH, a social and environmental epidemiologist at Harvard University, and colleagues explained that adults with Alzheimer’s disease and related dementias may be more susceptible to extreme heat for several reasons.
For example, compared with cognitively intact adults, “they may be slower to recognize symptoms of extreme heat exposure, or, if they recognize the symptoms, they may be less able to address them,” they wrote in JAMA Internal Medicine. “Because [Alzheimer’s disease and related dementias] affect thermoregulatory processes, adults living with [Alzheimer’s disease and related dementias] are more prone than others to heat-related illnesses, thus magnifying the potential impact of extreme heat.”
The researchers conducted a population-based cohort study to determine any links between extreme heat and hospitalizations among those with Alzheimer’s disease and related dementias by assessing 2000 to 2018 Medicare fee-for-service claims among beneficiaries aged 65 years or older.
They identified 3,329,977 first hospitalizations with Alzheimer’s disease and related dementias (63% women) during the study period.
Delaney and colleagues reported an OR for hospitalization with Alzheimer’s disease and related dementias on days in the 99th percentile of the heat index — the hottest 1% of days — vs. days in the 55th percentile of 1.02 (95% CI, 1.01-1.02) after 1 day of extreme heat exposure, equal to 0.8 (95% CI, 0.5-1.1) additional hospitalizations with Alzheimer’s disease and related dementias per 1,000 beneficiaries.
The researchers added that the lag-response curve showed that 1 day of extreme heat exposure raised hospitalization risk for 4 total days — “that is, on the initial day of exposure plus 3 additional lag days thereafter.”
They observed an OR for hospitalization with Alzheimer’s disease and related dementias after 4 days of continuous extreme heat exposure of 1.04 (95% CI,1.03-1.04), corresponding to 1.7 (95% CI, 1.3-2) additional hospitalizations with Alzheimer’s disease and related dementias per 1,000 beneficiaries.
The strength of effects of extreme heat exposure differed based on climates. Researchers calculated ORs for hospitalization after 3 days of continuous heat exposure of 1.05 (95% CI, 1.02-1.08) and 1.03 (95% CI, 0.99-1.08) in arid and tropical regions, respectively, but the latter region’s CI “included the null value,” Delaney and colleagues wrote.
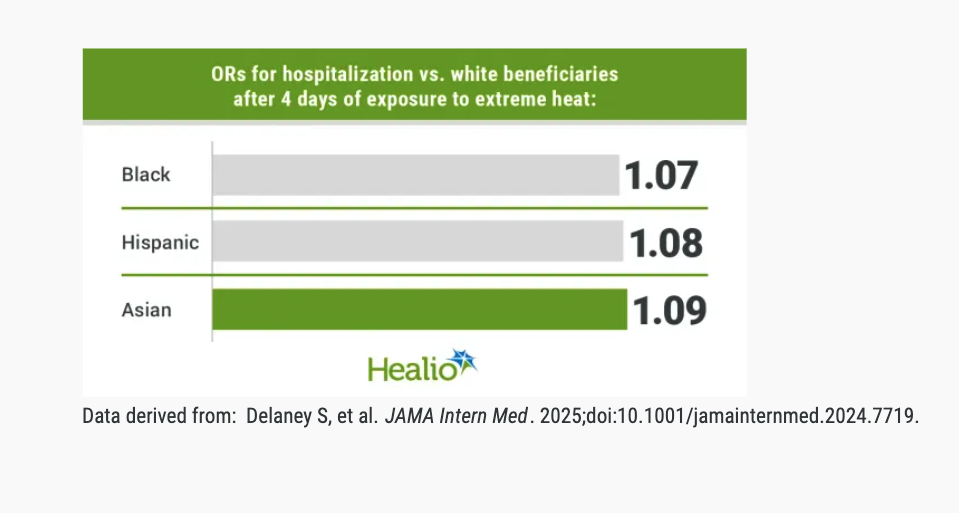
Compared with white beneficiaries, Black (OR = 1.07; 95% CI, 1.05-1.1), Hispanic (OR = 1.08; 95% CI, 1.03-1.13) and Asian (OR = 1.09; 95% CI,1.02-1.17) beneficiaries all had a greater risk for hospitalization with Alzheimer’s disease and related dementias after 4 days of continuous extreme heat exposure.
The researchers pointed out that extrapolating these findings to the estimated 6.7 million Americans living with Alzheimer’s disease and related dementias “suggests that each day of extreme heat could contribute to at least 5,360 added hospitalizations nationwide.”
They noted that historical and present-day policies, which have deprived diverse populations of resources like thermally comfortable housing, may contribute to the racial inequities observed.
“Many communities of color may also have less access to health care and fewer financial assets, which could be used to prevent effects of extreme heat,” they wrote.
Ultimately, there are several important takeaways for clinicians.
“At the patient level, educating patients and caregivers on the risk of extreme heat given [Alzheimer’s disease and related dementia]-related thermoregulatory deficits is important, particularly when patients require psychotropic medications,” Delaney and colleagues wrote. “Clinicians may also work with social service providers to ensure patients have adequate social support and access to air-conditioned spaces.”