Media representations of heatwaves and climate change play an important role in how the public thinks about, perceives, prepares for and acts on risks to their health, and how decision and policy makers address the problem.
The content on this page is intended to provide journalists, editors and others working in the media and communications sector with guidance and perspectives on how extreme heat and heat health narratives and imagery can help save lives and drive action.
Subscribe to our press list
Key Considerations
-
- Every heatwave and extreme heat event in the world is now made stronger and more likely because of human-induced global climate change. There is robust evidence that climate change is increasing the frequency, intensity, and duration of heatwaves worldwide, and these trends are projected to continue for the foreseeable future. Rising average temperatures also lead to increasing chronic heat risk.
- It is crucial that journalists and media frame stories about the impacts of rising heat within the context of climate change, both to connect the dots for the audience and to raise awareness that can help drive rapid climate action - addressing both mitigation and management options.
- Tip: Consult your National Meteorological Service before attributing heat events to specific global phenomena like El Niño.
-
- When covering ongoing extreme heat events, reference locally-relevant health advice and available resources. From how to access cooling or resilience centres to tips on low-cost cooling techniques, this information might just save lives.
- Consider highlighting resources that can help individuals and groups reduce their risk in the long-run, such as weatherization and home energy assistance programs or legal protections available to renters. Practical peer-reviewed information from authentic and reputed sources - such as The Lancet - can facilitate evidence-based actions.
- Specific guidance on actions to manage and adapt to heat at home, at work, in the environment, in the city, and in sports can also be found on our website.
-
- Heat impacts are not felt equally by everyone. People who are at increased risk, such as people with lower incomes and those who are unhoused or poorly housed, are often impacted well before risks become concerning for other populations. Many groups of people underestimate the dangers of heat and climate change more generally, both to themselves and for those under their care. The point at which heat becomes dangerous varies from one person to the next, with vulnerability and exposure being determined by individual and potentially compounding factors.
- Heat vulnerability factors may include lifestyle, living conditions, age, gender, culture, race and ethnicity, economic status, health status and medications, workplace health and safety protections, and access to resources and support. The exposure factors may include urban environment, building climatology and indoor conditions, prolonged heat exposure and behaviour, working hours, and acclimatisation.
- The voices of those most affected by heat should be amplified in reporting as a matter of climate justice using people-first language such as that suggested by the U.S. Centers for Disease Control and Prevention.
-
Heat doesn’t just harm health directly. It can alter human behaviour, the transmission of diseases, health service delivery, air quality, and critical social infrastructure such as energy, transport, and water. It can increase the risk of wildfires, ground-level ozone smog and flash floods. Hot weather, alone or in combination with other natural hazards, may exacerbate risks associated with mass gatherings (such as music concerts, and religious or sporting events), and disrupt emergency health services.
Practical Recommendations
Instead of waiting for an extreme heat event to begin or end before publishing coverage, create awareness in advance – both seasonally and before a projected heat event.
Raising public awareness around impending risks can enable them to take preventive action.
Instead of focusing only on high daytime temperatures, remind your audience that high nighttime temperatures can be extremely dangerous – even if it’s less hot than during the day – for those who don’t have adequate cooling at home.
Bodies need to continue working hard to cool down when temperatures remain elevated at night, which causes cumulative stress. Humidity and other factors can compound risk even after the sun goes down.
Instead of focusing on heat only in outdoor settings, remember that indoors can be hotter than outdoors, and excess indoor heat is deadly.
Environmental heat stress, exercise intensity and clothing are the three main sources of heat stress and impact people indoors at home, at work, and in institutions such as jails, schools and care homes. Indoor spaces may be poorly ventilated, workers may need to wear personal protective equipment, and buildings may have additional heat sources contributing to high temperatures.
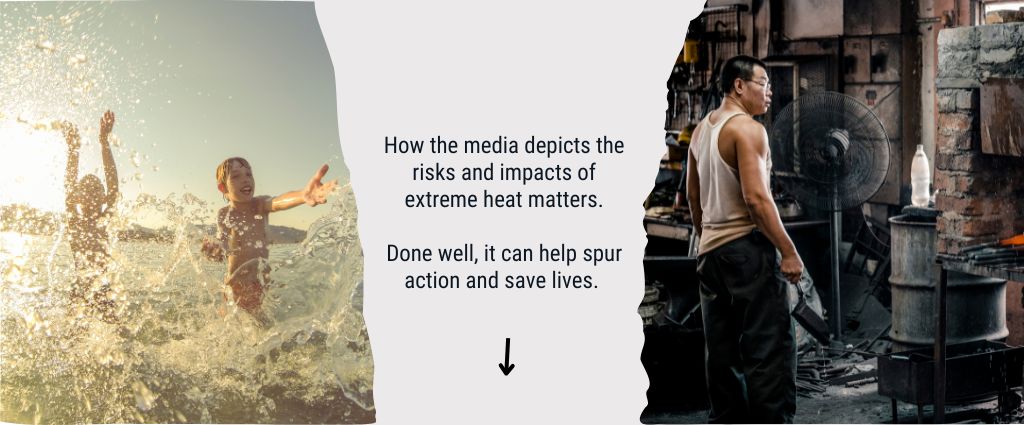
Instead of showing scenes of crowded beaches, swimming pools or fountains, show people struggling in the heat, and its negative and dangerous impacts.
Images that show people enjoying hot weather by spending time at the beach or pool hide the serious risk that many people face during hot weather, and often contradict the serious tone of the narrative. Negative impacts may include school closures, train cancellations due to buckled lines, impacts on food production, overrun ambulance services and ER waiting rooms, wildfires and air pollution, drought, flash flooding, etc.
Instead of only showing images of heat impacts, strike a balance by also showing positive action to mitigate or manage risk.
People tend to tune out excessively negative information, which can be perceived as alarmist. Instead, action-based imagery can provide a counter-message of hope and possibility to address the challenges of extreme heat. Positive action could include cooling centers, urban tree planting campaigns, home retrofitting grant initiatives, community outreach programmes that check on vulnerable populations, etc.
Instead of focusing only on heat stroke or mortality figures, look at the broad range of direct and indirect heat impacts on health and society.
Heat impacts manifest in many forms. Beyond mortality and morbidity figures, other areas worth exploring include impacts on labour productivity, stress, disease transmission, health service delivery, critical social infrastructure (including energy, transport, and water), congestion in hospitals, roads and public transit, car accidents, wildfires, ground-level ozone smog, flash floods, agricultural productivity and animal deaths, and outdoor exercise and exposure. Tip: Consider broader mortality figures, even if statistics are published months later.
Instead of focusing only on heatwaves, balance coverage between extreme heat events and chronic heat exposure and risk.
Chronic heat risk is increasing due to climate change and is a serious risk to health, particularly in hot climates worldwide where the majority of heat impacts occur outside extreme heat events.
Instead of conducting interviews only in hospital settings, find people where they are dealing with heat in various contexts.
Audiences want first-hand perspectives on how people are experiencing heat – at home, at work and in the community – and what they can do about it. Speak with the farm worker, gig worker, care home residents, ambulance driver, firefighter, and others.
Instead of only interviewing those in national or international expert roles, connect with local experts and researchers and responsible authorities.
Heat, health and climate change are global issues, but their impacts are felt locally. Heat risk varies greatly from location to location, and population to population. Heat and health experts who understand local conditions, perceptions and risk factors will provide an important perspective to the story, and can add to authoritative views from the national and international levels.
Instead of asking sources directly about heat and climate change,
ask about circumstantial factors that contribute to how they experience extreme heat.
The term ‘climate change’ and the idea that more extreme heat is being fuelled by it can evoke a strong response in some people, especially in areas with low acceptance of climate science or trust in the media,
While these people may be experiencing very real impacts of climate change, they may refute the connection. These sources will be more open to talk in terms that are less charged.
Instead of asking sources if they have experienced heat stroke or illness, ask sources if they’d experienced heat-specific symptoms.
The average person may not know the symptoms of heat illness, but will be able to explain how they are feeling – for example if they have experienced headaches, dizziness or cramps while working outside.
Interviews
Explore our online directory to identify experts by country, region and topic, or connect with our global Network management team for global perspectives and other requests.
Joy Shumake-Guillemot
Lead, WMO-WHO Joint Office for Climate and Health
World Meteorological Organization (WMO) and World Health Organization (WHO)
Topics: Big picture heat health overview, global heat action efforts and coordination
John Nairn
Extreme Heat Advisor, World Meteorological Organization (WMO)
Topics: The science behind heat and heatwaves. Meteorology.
Andreas Matzarakis
Head, Research Centre Human Biometeorology
German Meteorological Service (DWD)
Topics: Warning systems for health, human biometeorology, urban climatology, climate and tourism, micro-scale adaptation, German Heat Health Warning System
Julie Arrighi
Director (a.i.), Red Cross Red Crescent Climate Centre
Topics: Extreme heat risks for vulnerable populations, actions to reduce risk during an extreme heat event, adaptation measures to reduce future risks
Who we are
The Global Heat Health Information Network is a United Nations Initiative led by the World Health Organization (WHO), World Meteorological Organization (WMO), and US National Oceanic and Atmospheric Administration (NOAA). It is an independent, voluntary, and member-driven forum of scientists, practitioners, and policy makers focused on improving capacity to protect populations from the avoidable health risks of extreme heat in our changing climate.
Sources and Further Reading
- Global Heat Health Information Network
- Carbon Brief: Guest post: How heatwave images in the media can better represent climate risks. Saffron O’Neill (2019)
- CCNOW: Best Practices for Climate Journalism
- CCNOW: Your Guide to Making the Climate Connection
- CCNOW: Talking Shop: Covering the Human Impact of Extreme Heat
- World Weather Attribution: Reporting extreme weather and climate change: a guide for journalists
- International Public Opinion on Climate Change, 2022
Contributing Authors
Maddie West, WMO – WHO Joint Office for Climate and Health
Julie Arrighi, Red Cross Red Crescent Climate Centre / American Red Cross / University of Twente
Hunter Jones, National Integrated Heat Health Information System (NIHHIS), U.S. NOAA
Ladd Keith, University of Arizona
Kim Knowlton, NRDC / Columbia Mailman School of Public Health
Rupa Kumar Kolli, International Monsoons Project Office, Indian Institute of Tropical Meteorology
Andreas Matzarakis, Research Centre Human Biometeorology, German Meteorological Service
Jason Lee, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
Chao Ren, Faculty of Architecture, The University of Hong Kong
Audrey Tan, Centre for Nature-based Climate Solutions, National University of Singapore, Singapore
Abhiyant Tiwari, NRDC India
